Medication Prescribing for Older Adults
INTRODUCTION
Persons over age 65 represent about 12% of the population, yet they receive over 25% of all prescribed drugs in the United States.1 One national survey showed that 50% of community-dwelling elderly over age 65 used five or more prescription and over-the-counter (OTC) medications per week, and 12% used 10 or more.2 Thirty percent of hospital admissions in elderly patients can be linked to adverse drug events, defined as “noxious and unintended patient events (ie, symptoms, signs, and laboratory abnormalities) caused by a drug.” The most common cause of adverse drug events is inappropriate medication prescribing.3
Medications are deemed to be inappropriate if they pose more risk than benefit to the individual. The risk of adverse drug events resulting from inappropriate medication prescribing range from weakness, to falls and fractures, to even life-threatening events.4,5 Studies show prevalence of at least one inappropriate medication being prescribed for up to 40% of nursing home residents and 21% of community-dwelling elderly.6
Underprescribing of medically indicated drugs such as low-dose aspirin can also place a person at risk. Suboptimal prescribing has been shown to adversely impact outcomes for many diagnoses, including cardiovascular disease, stroke prevention, and osteoporosis prevention.7-9 Underuse of medications can result from fear of prescribing a medication that might lead to adverse events, attempts to prevent polypharmacy, economic barriers, or lack of patient adherence to medications.10 Thus, providers must balance the pros and cons of each medication that they prescribe for their older patients.
Achieving adherence to needed medications can be challenging.11 Factors affecting adherence that are disproportionately represented in the elderly include polypharmacy, polydosing, cognitive deficits, and impaired physical function. Lack of adherence to prescribed medicines increases the likelihood of an adverse outcome, including treatment failure, medication overdose, and avoidable hospitalization.12
PHYSIOLOGIC CHANGES WITH AGING
Pharmacokinetics refers to drug absorption, distribution, metabolism, and elimination. While drug absorption is typically slowed but complete in the elderly, aging has profound affects on distribution, metabolism, and excretion of drugs. Volume of distribution of medications is decreased by the reduced muscle mass and total body water typical of aging. As a result, medications will attain higher plasma concentrations if they distribute into muscle or total body water. This is particularly important for medications that require loading doses. Another typical change with aging is increased fat mass, which acts as a depot for lipophilic drugs such as benzodiazepines and amiodarone.13
Drug potency and duration of action are often increased in the elderly due to decreased renal and hepatic function. The Cockroft-Gault formula should be used to estimate creatinine clearance in older adults when prescribing a new medication or when changing doses:
Creatinine clearance = (140-age) x weight (kg) (x 0.85 for women)
72 x serum creatinine
Serum creatinine does not accurately reflect renal function in older persons because of decreased lean body mass.14
COMMON CHARACTERISTICS OF OLDER ADULTS WITH MEDICATION-RELATED PROBLEMS
In addition to physiologic changes of aging, the accumulation of medical diagnoses also contributes to medication-related problems. Certain patient characteristics should prompt the provider to pay special attention to potential prescribing problems. Persons at particular risk are over age 85, take nine or more medications or more than 12 doses of medication per day, or have at least six active chronic medical diagnoses, especially renal impairment.15
MEDICATIONS COMMONLY LEADING TO ADVERSE EVENTS: BEERS CRITERIA
The Beers criteria is one of the most widely used consensus criteria for appropriate medication use in the elderly patient population.16 Originally developed in 1991 for the nursing home setting, the criteria were updated in 1997 to include all geriatric patients regardless of setting.17 The Beers criteria were last updated in 2003 to include new evidence on the pharmacologic changes associated with aging and its impact on safety and effectiveness.18 The list of criteria was developed by a national panel of experts in geriatric care and pharmacology to include 48 medications or classes of medications to avoid in individuals age 65 or older, and 20 medications that should not be used in older persons known to have specific conditions. Drugs are deemed inappropriate for use among the elderly population due to:
• Lack of proven efficacy, high likelihood of adverse drug effects, potential for severe effects, or a high potential for an interaction with another medication or class of drug
• Specific medications or classes of medications that should not be used routinely in elderly patients with specific disease states
• Specific medications that pose a serious risk of causing an adverse event when safer alternatives are available
• High doses of certain medications
• Excessive dosing frequencies, which complicate compliance for elderly patients
• Extended duration of medications that were intended to be used for a limited time
Table I, adapted from the 2003 Beers criteria, details common medications that can potentially lead to a serious adverse event in elderly patients. Most of the medications listed in the table are to be avoided in those over the age of 65, while others such as short-acting benzodiazepines, fluoxetine, and digoxin are appropriate at lower doses. Many drugs classified as inappropriate for elderly persons produce minor anticholinergic effects such as dry mouth, constipation, and blurred vision. More serious anticholinergic symptoms such as hypotension, cardiac arrhythmias, urinary retention, and confusion can also occur. In general, agents that cause anticholinergic properties should be avoided in this vulnerable population.19
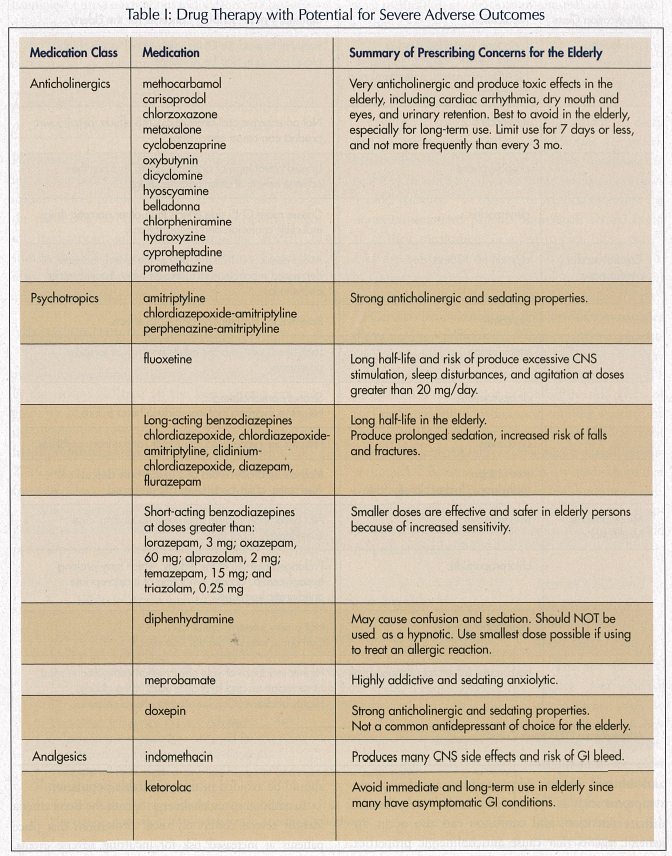
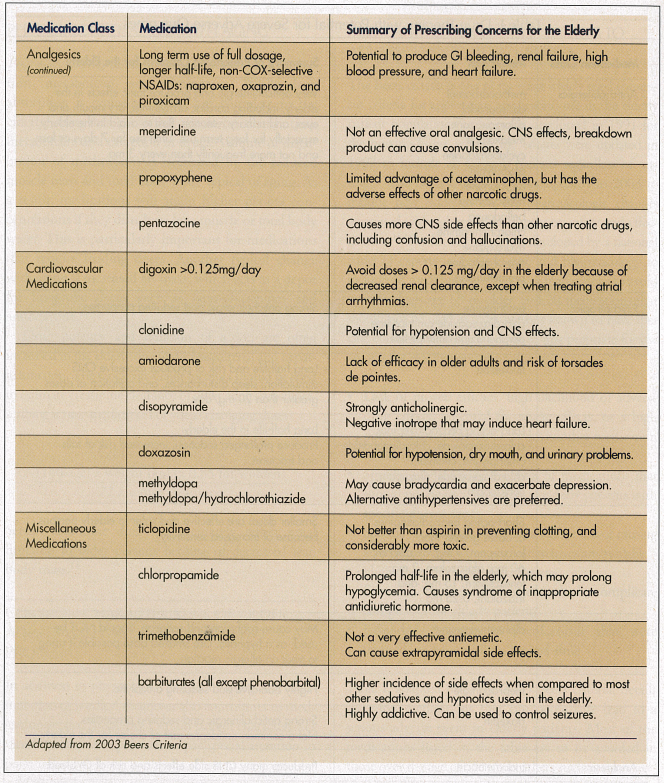
In addition to anticholinergic agents, the Beers criteria identify several commonly used medications that place patients at increased risk for incurring adverse events. Examples of these medications include long-acting benzodiazepines, amiodarone, doxazosin, diphenhydramine, meperidine, propoxyphene, and long-term use of full dose nonsteroidal anti-inflammatory drugs (NSAIDs).20-22
APPROACH TO MEDICATION PRESCRIBING AND MANAGEMENT FOR OLDER PERSONS
Polypharmacy and inappropriate medication prescribing are key issues for older persons. Reduction of medication-related problems in the elderly can take place at the point of initial prescribing, when reviewing ongoing medications, and when determining whether to stop medications. Involvement of the entire health care team, including the pharmacist and caregiver, can play a role in medication prescribing and adherence.
Medication Prescribing and Review
At the point of initial prescribing, it is important to avoid using medications that are potentially inappropriate in the elderly. Reliance on the Beers criteria can help guide use of medications associated with the least risk for the elderly. The Beers criteria can be accessed online at archinte.ama-assn.org/cgi/reprint/163/22/2716.pdf or downloaded to a PDA at freewarepalm.com/medical/beers’list.shtml.
When starting a new medication, use the lowest possible dose and titrate slowly. A rule of thumb to help prevent potentially harmful iatrogenic illness is to initiate a medication at one-third to one-half of the manufacturer’s recommended dosage.23 Whenever possible, once-a-day dosing is preferred since complex dosing makes it difficult for patients to adhere to medications.24 Table II describes a general approach to medication prescribing in the elderly.
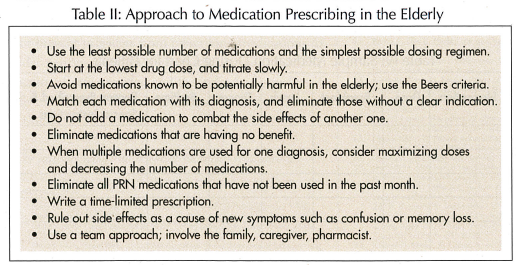
Healthcare providers have an opportunity at every visit to review and withdraw medications as needed. Healthy People 2010, a national initiative to improve the health of Americans, calls for regular medication reviews in older patients.25 To assist in the medication review for noninstitutionalized patients, individuals should bring all of their medications in a bag to each office visit.26 Likewise, for patients who may be cognitively impaired, it is important to review the medications with the person responsible for administering them.27
Certain circumstances can alert providers to consider discontinuing medications. When a patient presents with new signs or symptoms, consider whether the symptoms might be a result of current drug therapy. If a medication is being added to combat the side effects of previously prescribed medications, consider whether the first medication truly warrants use. If a medication is not improving patient health or comfort, it should be discontinued.28 Be attuned to unnecessary medications that may linger following transitions in level and site of care. Multidisciplinary geriatric assessments can reduce inappropriate drug use and underuse in the inpatient and outpatient setting.29
Use of OTC and Complementary Medications in the Older Adult
The use of OTC agents and herbal preparations adds to the challenge of prescribing appropriate medications for older patients. The presence of polypharmacy puts elderly persons at risk for herb-drug interactions. Over the past decade, the use of OTCs has been increasing, with 31-96% of adults age 65 and older using them. The most commonly used classes of OTC medications include analgesics, laxatives, and vitamins and minerals.30 A national survey found that 12.9% of elderly persons had used an herbal product in the last year, such as glucosamine, echinacea, and garlic. Less than half of users discussed their herbal supplements with providers.31 Due to the high prevalence of these agents in the elderly population, providers need to include nonprescription medications in the medication review.
Prescribing Issues Unique to the Long-Term Care Setting
Healthcare providers face a unique set of challenges when prescribing medications to older residents in the long-term care setting.32 In this highly regulated setting, use of more than nine medications, including OTC products such as vitamins and calcium supplements, is considered polypharmacy.33 These residents are at high risk for hospitalization and often have multiple specialists involved in their care. Transitions of care and multiple prescribers pose risks to maintaining an accurate and appropriate list of medications. For example, upon return from a hospitalization, newly prescribed proton pump inhibitors or histamine blockers should be discontinued unless there is a clear indication. Likewise, after recovering from a COPD exacerbation, it is important to discontinue any “forgotten” steroids. Providers need to remember to discontinue medicines not central to patient comfort when the decision for palliative care or hospice is made.34
Improving Medication Adherence
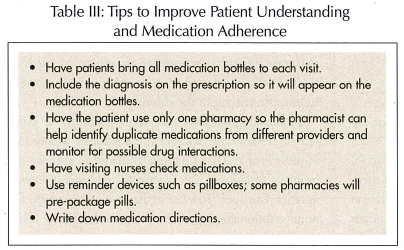
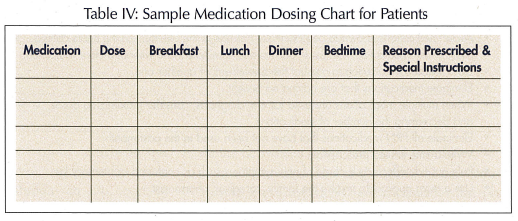
Achieving medication adherence is a particularly important issue for elderly persons who are still managing medications independently. Medication adherence rates are as low as 50% for chronic conditions.35 Lack of adherence can be attributed to complicated regimens, lack of understanding, physical and cognitive deficits, anticipation of side effects, and financial obstacles.36,37 A number of strategies can be used to try to improve medication adherence (Table III). Initially and with regimen changes, the patient should be given a complete list of his or her medications, including why they are taking them38 (Table IV). Coordinate with the caregiver, pharmacy, and other providers. Use of reminder devices such as pillboxes can benefit some patients.39 If a patient is having adherence issues, a home care consult can help to assess the situation.
Broader Strategies to Improve Prescribing
In addition to the endeavors of the individual provider, institutions have a role in improving prescribing and adherence by instituting elder-friendly formularies and protocols.40 Computerized physician order entry and electronic health records can flag potential medication risks and drug interactions.41 Challenges beyond the level of the institution are the large number of insurance company formularies, including the new Medicare Part D prescription drug plan. In order to systematically address medication prescribing issues, improved infrastructures within both the office and long-term care settings need to be explored. On a broader level, older persons, including the institutionalized elderly, need to be included in clinical trials to assess safety and efficacy of medications in this population.
CONCLUSION
Persons over age 65 use more medications than their younger counterparts. The combined effect of aging and polypharmacy places older persons at increased risk for adverse drug events, some of which are preventable. To improve outcomes, it is important to eliminate unnecessary medications and restrict medications to those with proven efficacy and the least chance of adverse drug effects. Using an evidence-based resource such as the Beers criteria can assist in medication prescribing. Caution is advised when prescribing any medication for this vulnerable population. Due to the potential for adverse drug events, the healthcare team needs to regularly review medication regimens and opportunities to withdraw unnecessary medications. At the same time, desire to reduce polypharmacy should not prevent providers from prescribing medications to older persons when they are medically indicated. The quality of care provided and the individual’s quality of life may be significantly enhanced by improved prescribing.
The authors report no relevant financial relationships.









